GAIT: NORMAL, ABNORMAL & ASSESSMENT - ppt download
$ 16.50 · 4.7 (729) · In stock
GAIT 1- Normal Walking 2- Gait cycle – phases, temporal parameters 3- Determinants of gait 4- Kinematic & kinetic analysis 5- Gait in young, elderly & women 6- Some abnormal gaits 7- Assessment – visual, video recording 8- Clinical Gait laboratory
Dr Raj Kumar Yadav. MBBS, MD (PMR) Assistant Professor, PMR.
3- Determinants of gait. 4- Kinematic & kinetic analysis. 5- Gait in young, elderly & women. 6- Some abnormal gaits. 7- Assessment – visual, video recording. 8- Clinical Gait laboratory.
- it’s advancement in the desired line of progression. Muscle act - this motion and forces are controlled. Normal walking – - weight bearing stability and. progression over the supporting foot. optimal conservation of physiologic energy.
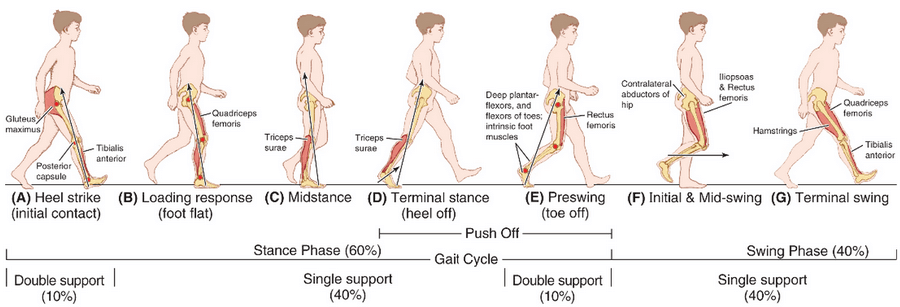
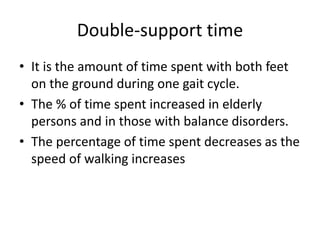
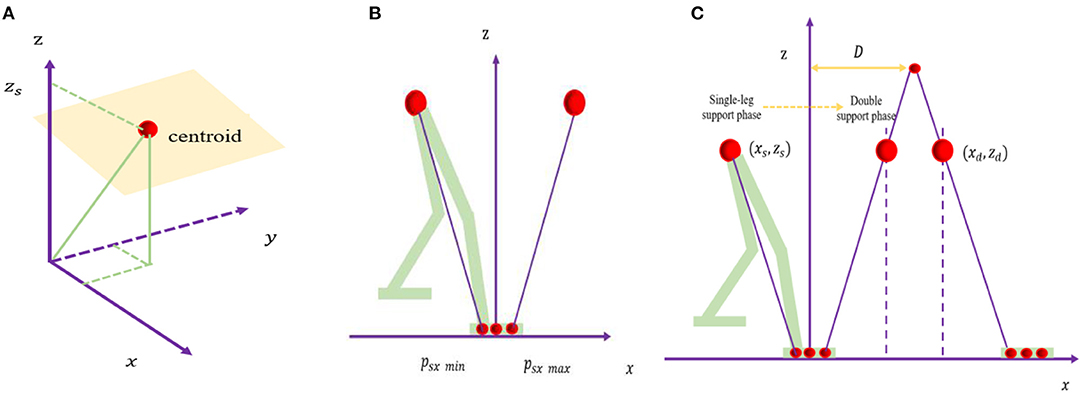
STANCE PHASE :- Phase in which limb is in contact with the ground. (60%) SWING PHASE :- Phase in which the foot is in air for limb advancement. (40%) DOUBLE SUPPORT: When two extremities are in contact with the ground simultaneously. - cadence (speed of walking) - double support. - Absence of double support - running.
immediately following initial contact - lift of C/L extremity from ground. weight shift occurs.
Mid- stance: (11-30%) - lift of C/L extremity from ground - ankles of both extremities are aligned in the frontal (coronal) plane. Terminal stance: (30-50%) - ankle alignment in frontal plane - just prior to initial contact of C/L extremity. Preswing: (50-60%) - initial contact of C/L extremity - prior lift of Ipsilateral extremity from ground.
Initial swing: (60-73%) Lift of the extremity from ground - position of maximum knee flexion. Mid swing: (73-87%) Immediately following knee flexion - vertical tibia position. Terminal swing: (87-100%) Following vertical tibia position - just prior to Initial contact.
Stride length: Linear distance between corresponding successive points of contact of the same foot. Highly variable - normalized by dividing it by leg length or total body height. increases as the speed increases. Step length: opposite foot. - gait symmetry.
Velocity (meters/minute): Distance covered in given time in the given direction. Step width (width of walking base): Distance between the midpoints of the heel of two feet. increases - increased demand for side to side stability.
Angle between the line of progression and the line intersecting the centre of heel and the second toe. decreases as the speed increases.
Average value. Velocity (m/s) 0.9 – 1.5. Cadence (steps/min) Stride length (m) 1 – 1.5. Step length (cm) 38. Walking base (cm) Degree of toe-out. 7º. Stance phase. 60% Swing phase. 40% Double limb support. 20%
Optimizations to minimize excursion of centre of gravity (COG), hence reduction of energy consumption. Pelvic rotation. Pelvic tilt. Knee flexion in stance. Ankle PF. Foot supination. Lateral displacement of the pelvis. Determinants reduce displacement on the vertical plane (50%) determinant 6 - horizontal plane (40%).
equal but opposite. GRFVector = sum of the force components in each direction (vertical, anteroposterior and mediolateral axes) typical pattern from initial contact to toe-off. MOMENTS (Torque/ turning force)- External forces - GRF, gravity and inertia - external moments about the joints. Internal moments - moments generated by the muscles, joint capsules, and ligaments - countract the external forces.
Kinetics : Study of forces, moments, masses and accelerations, but without any detailed knowledge of the position or orientation of objects involved. Kinematics : Describes motion, but without reference to forces involved.
Total excursion of trunk is 7° and pelvic girdle 12°. Total ROM of shoulder is 30° (24° of extension and 6° of flexion) Center of gravity (COG) is located 5 cm anterior to second sacral vertebra. It is displaced 5 cm horizontally and 5 cm vertically during a gait cycle.
Whole leg is externally rotated during swing phase (2 yr) Walking base is wider (4 yr) Absence of reciprocal arm swing (4 yr) Stride length and velocity are lower and cadence higher (15 yr)
Decreased stride length and cadence. Increase in walking base. Reduction in total range of flexion and extension of joints. GAIT IN WOMEN. Gait speed is slower. Step length is smaller. Increased cadence.
motor system. skeletal supports. neural control. combination of the above.
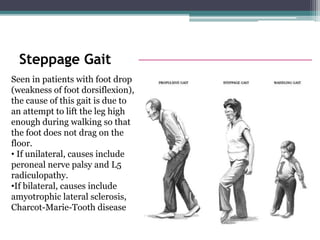
weakness of ankle dorsiflexors. excessive knee and hip flexion with toes pointing downwards in the swing phase. Avoidance of weight bearing on the affected limb. shortening of stance phase in that limb.
The knee is hyper-extended and locked at end of stance phase and entire swing phase. So to clear the leg the patient goes up on the toes of the other leg to clear the affected limb.
The gluteus medius during the stance phase, pulls the stance side pelvis over the supporting limb to prevent excessive pelvic drop in the opposite swing limb. If the hip abductors are weakened, the opposite limb pelvis may drop excessively during swing phase. To avoid this, the entire trunk shifts to the stance side to bring the stance pelvis on to the supporting limb. This is known as gluteus medius lurch or trendelenburg gait.
If both hip abductors are weak, the trunk sways from side to side during the stance phase to bring the pelvis level on the supporting limb. waddling gait. muscular dystrophies. accompanied by excess lumbar lordosis to compensate for hip extensor weakness.
heel strike is missing and patient lands on forefoot. Since hip and knee are kept extended throughout the gait cycle, there is relative limb lengthening and hence circumduction or hip hiking is used for clearance. Toe drag may be present in swing phase. Swing phase is longer on the affected limb. Decreased arm swing on the affected side. If flaccid paralysis or flexor synergy is present. knee buckling and instability.
Lack of arm swing. Short, quick steps with increasing speed. Cannot stop abruptly or change directions. Stooped posture. Seen in. Parkinsonism. Carbon monoxide poisoning.
Staggering and lack of smooth movements (reeling or drunken gait) Falls to the side of lesion. Compensated by wide-based gait to increase base of stability.
Gait with heavy heel strikes, forceful knee extension and improper foot placement as well as a postural instability. Usually worsened when the lack of proprioceptive input cannot be compensated for by visual input, such as in poorly lit environments. Friedreich’s ataxia, pernicious anemia, tabes dorsalis, spinal cord pathologies.
Hip and knee increased flexion throughout stance with ankle dorsiflexion. Due to hamstring tightness. Jump knee gait. Flexion at hip and knee and ankle equinus is characteristic of this gait.
excess knee extension throughout swing. Has to use circumduction or vaulting. Due to increased rectus femoris activity in swing phase. Recurvatum knee. Due to triceps spasticity or hamstrings transfer. Leads to increased knee extension in mid & late stance.
rigidity and excessive adduction of the leg in swing. plantar flexion of the ankle. increased flexion at the knee. adduction and internal rotation at the hip. Diplegic CP, Spinal cord pathologies.
Symmetry and smoothness of movements. Balance. Degree of effort. Motion of specific segments. Gait parameters. Gait should be observed from at least 3 angles (side, front & back)
depends entirely on the skill of the individual observer. Gait analysis walkway. Length – m. Width - visual - 3 m. video recording - 4 m. kinematic system - at least 6 m.
Advantages- gives permanent record. can observe high speed events. reduces the number of walks a subject needs to do. makes it possible to show the subject exactly how they are walking. makes it easier to teach visual gait analysis to someone else. The majority of today’s domestic cameras are perfectly suitable for use in gait analysis.
A fully equipped clinical gait laboratory can be expected to posses a combined kinetic/kinematic systems, with ambulatory EMG, as well as facilities for making videotapes. Equipment may also be available for measuring oxygen uptake or pressure beneath the feet.
- Usual methods of displaying force platform data is the butterfly diagram.
EMG measures the electrical activity of a contracting muscle during different phases of gait cycle. 1- Surface electrodes- Not suitable for deep muscles like iliopsoas. 2- Fine wire electrodes- 3- Needle electrodes-
Oxygen consumption- measurements of oxygen uptake. while not particularly pleasant for the subject (who has to wear face mask or mouth piece) Practical. Whole body calorimetry- most accurate way but quite impractical. subject is kept in an insulated chamber for measuring the heat output of the body. Physiological Cost Index: less accurate. PCI = (Walking HR – Resting HR) Walking Speed in m/min.

PPT) GAIT Dre Jon

Download Free Medical Approach to Abnormal Gait PowerPoint Presentation
Gait Training : Normal Gait Pattern ,Abnormal Gait , Exercises

Using and interpreting electrodiagnostic tests
PPT - DISORDERS OF GAIT PowerPoint Presentation, free download - ID:5318168

From heart to muscle: pathophysiological mechanisms underlying long-term physical sequelae from SARS-CoV-2 infection
Gait abnormalities presentation

Gait normal & abnormal

PPT – Intoeing, Outtoeing, and LimpingMaking Sense of Common Pediatric Gait Abnormalities PowerPoint presentation

Gait
Total Hip Replacement: 3 Exercises for an Earlier Return of Functional Gait - MedBridge Blog
partB GaitMechanics.ppt







:quality(85):upscale()/2024/02/22/945/n/1922729/1780ab7965d7bfa9cce0a2.81891219_.jpg)